Heart catheterisation remains one of the most frequently performed cardiovascular procedures worldwide, yet many patients experience significant anxiety about potential discomfort during the intervention. This minimally invasive diagnostic and therapeutic procedure involves threading thin, flexible catheters through blood vessels to reach the heart, enabling cardiologists to assess cardiac function, diagnose conditions, and perform treatments. While advances in anaesthetic techniques and procedural refinements have substantially improved patient comfort, understanding the pain experience during catheterisation helps patients prepare mentally and physically for the procedure. The reality is that most patients experience minimal discomfort during heart catheterisation, with local anaesthesia effectively managing pain at insertion sites and modern sedation protocols addressing anxiety-related concerns.
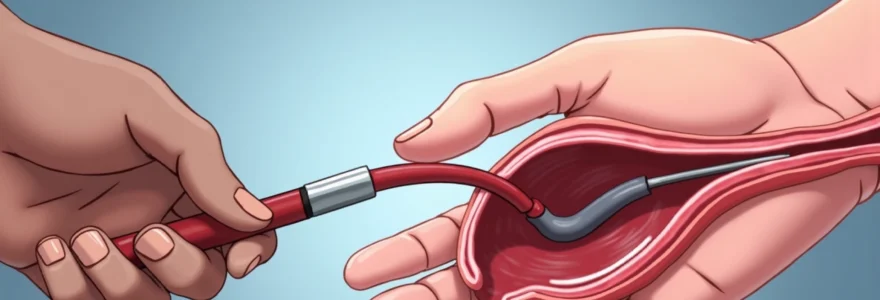
Cardiac catheterisation procedure: percutaneous coronary intervention and diagnostic angiography
Modern cardiac catheterisation encompasses both diagnostic angiography and therapeutic interventions, with the procedure’s complexity directly influencing patient comfort levels. During diagnostic catheterisation, cardiologists insert thin catheters through arterial or venous access points to visualise coronary arteries, assess cardiac pressures, and evaluate heart function. The procedure typically begins with meticulous sterile preparation of the access site, followed by local anaesthetic administration to ensure patient comfort throughout the intervention.
The catheter insertion process involves creating a small puncture in the chosen blood vessel, typically measuring 2-3 millimetres in diameter. Most patients describe the initial needle insertion as similar to a blood draw, with the local anaesthetic providing effective pain relief within seconds. The catheter advancement through blood vessels is generally painless , as blood vessels lack the nerve endings that would register discomfort. However, patients may experience pressure sensations or awareness of the catheter’s presence without actual pain.
Transfemoral versus transradial access site selection
The choice between femoral and radial artery access significantly impacts patient comfort during and after catheterisation. Transfemoral access, utilising the large femoral artery in the groin region, traditionally served as the gold standard approach but requires post-procedural bed rest to prevent bleeding complications. Many patients find the groin puncture more uncomfortable initially, as this area contains numerous nerve endings and the larger needle size necessary for femoral access can cause more sensation during insertion.
Transradial access, performed through the radial artery at the wrist, has gained popularity due to enhanced patient comfort and reduced complications. The radial approach eliminates the need for prolonged bed rest, allowing immediate mobilisation post-procedure. Patients consistently report greater satisfaction with radial access , citing reduced discomfort during insertion and improved comfort during recovery. However, radial access may not be suitable for all patients, particularly those with small radial arteries or previous radial interventions.
Fluoroscopic guidance and contrast media administration
Fluoroscopic imaging provides real-time visualisation during catheter navigation, enabling precise positioning without patient discomfort. The X-ray exposure during fluoroscopy is minimal and painless, though patients must remain still during imaging sequences. Contrast media injection represents a unique aspect of the catheterisation experience, often producing distinctive sensations that patients should anticipate.
When contrast dye enters the coronary circulation, most patients experience a warm, flushing sensation that spreads throughout the body. This feeling, while initially surprising, is completely normal and typically lasts 10-15 seconds. Some patients describe a metallic taste or the sensation of having “wet themselves,” which results from the contrast affecting nerve receptors. These sensations are temporary and not indicative of complications , though forewarning patients about these expected effects reduces anxiety significantly.
Intravascular ultrasound and optical coherence tomography applications
Advanced imaging techniques during catheterisation, including intravascular ultrasound (IVUS) and optical coherence tomography (OCT), provide detailed vessel wall assessment without additional patient discomfort. These imaging catheters are extremely thin and cause no additional pain beyond the initial access site preparation. IVUS utilises sound waves to create detailed cross-sectional images of blood vessel walls, while OCT employs light waves for high-resolution vessel imaging.
The integration of these advanced imaging modalities into routine catheterisation procedures has improved diagnostic accuracy without compromising patient comfort. Most patients remain unaware when IVUS or OCT imaging occurs, as these techniques operate through the same catheter system used for standard angiography. The additional procedural time required for advanced imaging rarely exceeds 10-15 minutes.
Coronary angioplasty and stent deployment techniques
When therapeutic intervention becomes necessary during catheterisation, procedures such as balloon angioplasty and stent deployment may cause temporary chest discomfort. During balloon inflation to open blocked arteries, patients often experience chest pressure or tightness similar to their original symptoms. This discomfort results from temporary interruption of blood flow during balloon inflation and typically resolves immediately upon balloon deflation.
Stent deployment, involving the permanent placement of small metal mesh tubes to maintain arterial patency, usually causes minimal additional discomfort. The rapid deployment process, completed within seconds, produces brief chest pressure that quickly subsides. Modern drug-eluting stents are designed for comfortable deployment with minimal vessel trauma, contributing to reduced patient discomfort during the procedure.
Local anaesthesia protocols: lidocaine administration and sedation options
Contemporary anaesthetic protocols for cardiac catheterisation prioritise patient comfort through comprehensive local anaesthesia and tailored sedation strategies. Lidocaine remains the gold standard local anaesthetic for catheterisation procedures, providing reliable pain relief at access sites within 30-60 seconds of administration. The initial lidocaine injection causes a brief stinging sensation, often described as similar to dental anaesthesia, followed by complete numbness of the insertion area.
Proper local anaesthetic technique involves layered administration, beginning with superficial skin infiltration and progressing to deeper tissue planes. This approach ensures comprehensive numbness throughout all tissue layers that the catheter will traverse. Experienced operators allow adequate time for anaesthetic onset, typically 2-3 minutes, before proceeding with arterial puncture. The effectiveness of local anaesthesia means that most patients experience no pain during catheter insertion, advancement, or manipulation.
The goal of modern catheterisation anaesthesia is to ensure complete patient comfort while maintaining consciousness for procedural cooperation and immediate post-procedural assessment.
Topical benzocaine application for arterial access
Some catheterisation laboratories employ topical anaesthetic agents, such as benzocaine gel, as an adjunct to local infiltration anaesthesia. Applied 10-15 minutes before the procedure, topical anaesthetics begin surface numbing before needle insertion, potentially reducing discomfort from the initial local anaesthetic injection. However, topical agents alone provide insufficient anaesthesia for arterial puncture and require supplementation with injectable local anaesthetics.
The combination of topical and injectable anaesthesia creates a virtually painless insertion experience for most patients. This dual approach particularly benefits anxious patients or those with previous negative experiences with medical procedures. The additional preparation time required for topical anaesthetic application is minimal and often coincides with other procedural preparations.
Conscious sedation using midazolam and fentanyl
Conscious sedation protocols utilise medications such as midazolam for anxiolysis and fentanyl for analgesia, creating a relaxed, comfortable state while maintaining patient responsiveness. Midazolam, a short-acting benzodiazepine, reduces anxiety and creates mild amnesia, helping patients feel calm throughout the procedure. The medication’s rapid onset and relatively short duration make it ideal for outpatient catheterisation procedures.
Fentanyl supplementation provides additional pain relief beyond local anaesthesia, particularly beneficial for complex or prolonged procedures. The combination of these medications creates profound patient comfort while preserving the ability to follow instructions and communicate with the medical team. Careful dosing based on patient age, weight, and medical history ensures optimal sedation without respiratory depression or excessive drowsiness.
Regional nerve blocks for radial artery catheterisation
For transradial catheterisation, some operators employ regional nerve blocks targeting the radial nerve to enhance patient comfort. These blocks provide superior anaesthesia compared to local infiltration alone, particularly for complex cases requiring prolonged catheter manipulation. The ultrasound-guided technique allows precise anaesthetic placement around the radial nerve, ensuring comprehensive numbness throughout the procedural area.
Regional blocks offer extended post-procedural pain relief, reducing discomfort during the recovery period when local anaesthetics wear off. This approach proves particularly valuable for patients undergoing complex interventional procedures or those with heightened pain sensitivity. The additional time required for nerve block placement is often offset by improved patient comfort and cooperation during the procedure .
Pain assessment during catheter insertion and guidewire navigation
Understanding the pain experience during different phases of catheterisation helps both patients and healthcare providers optimise comfort strategies. The initial arterial puncture represents the moment of greatest potential discomfort, though proper local anaesthesia typically reduces this to minimal pressure sensation. Patients often report feeling the needle “pop” through the arterial wall, a tactile sensation rather than true pain when adequate anaesthesia is achieved.
Guidewire insertion and catheter advancement through blood vessels generate minimal discomfort in most patients. The blood vessels themselves contain few pain receptors, making catheter navigation generally painless. However, some patients experience awareness of the catheter’s presence, describing sensations of “movement” or “pressure” without actual pain. These sensations are normal and typically fade as patients become accustomed to the catheter’s presence.
Catheter manipulation within the heart chambers occasionally produces brief palpitations or rhythm irregularities that patients may perceive as uncomfortable. These temporary arrhythmias result from mechanical stimulation of cardiac tissue and resolve immediately when the catheter is repositioned. Patients should be reassured that these sensations, while noticeable, are expected and not dangerous.
Pain assessment during catheterisation utilises standardised scales, typically ranging from 0-10, with regular monitoring throughout the procedure. Most patients report pain scores of 2-3 during access site preparation and 0-1 during catheter manipulation. Higher pain scores usually indicate inadequate local anaesthesia or patient anxiety , both of which can be addressed immediately with additional medication or reassurance.
Post-procedural discomfort: haematoma formation and vascular complications
The post-procedural period presents distinct comfort considerations, with most discomfort arising from access site healing rather than cardiac effects. Immediate post-catheterisation care focuses on achieving haemostasis at the puncture site through manual compression or closure devices. Manual compression, typically lasting 10-20 minutes for arterial access, can cause significant discomfort due to the sustained pressure required to achieve bleeding control.
Haematoma formation represents the most common source of post-procedural pain, occurring in approximately 2-5% of cases despite careful technique. Small haematomas cause localised tenderness and bruising, while larger collections may produce significant pain and swelling. Most haematomas resolve spontaneously within 1-2 weeks, with pain management through oral analgesics and ice application during the acute phase.
Vascular complications, though rare, can cause considerable discomfort when they occur. Pseudoaneurysm formation, affecting less than 1% of patients, creates a pulsating mass that may cause pain and require intervention. Arteriovenous fistula formation can produce uncomfortable thrill sensations and may require surgical repair. Early recognition of these complications through careful monitoring prevents progression to more serious sequelae .
Post-procedural comfort depends largely on meticulous technique during the initial procedure and appropriate aftercare protocols tailored to individual patient needs.
Bed rest requirements following femoral access contribute significantly to post-procedural discomfort, particularly for elderly patients or those with mobility issues. The typical 4-6 hour flat bed rest period can cause back pain, hip discomfort, and general restlessness. Transradial access eliminates these positioning requirements, allowing immediate mobilisation and significantly improving patient satisfaction scores.
Patient experience variations: age demographics and comorbidity factors
Patient age significantly influences pain perception and tolerance during cardiac catheterisation, with distinct patterns observed across different demographic groups. Younger patients often experience greater anxiety about the procedure but typically tolerate physical discomfort better than elderly counterparts. Their robust vascular systems allow easier catheter manipulation with reduced procedural complexity and duration.
Middle-aged patients, representing the largest catheterisation demographic, generally demonstrate realistic expectations and good procedural tolerance. This group often benefits from detailed procedural explanations and active participation in comfort decisions, such as sedation preferences and positioning options. Their ability to communicate effectively during the procedure enables real-time comfort adjustments.
Comorbidity factors substantially impact the catheterisation pain experience, with conditions such as peripheral arterial disease potentially complicating catheter insertion and navigation. Patients with severe atherosclerotic disease may experience more discomfort during guidewire advancement due to vessel tortuosity and calcification. These technical challenges can prolong procedures and increase patient discomfort despite optimal anaesthetic management.
Elderly patients and Osteoarthritis-Related positioning difficulties
Elderly patients face unique comfort challenges during catheterisation, particularly related to positioning requirements and age-related physiological changes. Osteoarthritis commonly affects this population, making prolonged supine positioning uncomfortable even before procedural considerations. The standard catheterisation table, while necessary for procedural requirements, may exacerbate existing joint pain and stiffness.
Age-related skin changes increase bruising susceptibility and may prolong healing at access sites. Elderly patients often require additional padding and positioning support to maintain comfort during procedures. Careful attention to pressure points and frequent position adjustments can significantly improve the elderly patient experience without compromising procedural safety or efficacy.
Diabetic neuropathy impact on pain perception
Diabetic neuropathy creates complex pain perception patterns that can both mask and exaggerate discomfort during catheterisation. Peripheral neuropathy may reduce sensation at access sites, potentially requiring adjusted local anaesthetic dosing to account for altered nerve function. Conversely, some diabetic patients experience heightened sensitivity to certain stimuli, necessitating individualised comfort strategies.
The unpredictable nature of neuropathic pain responses requires careful monitoring and flexible anaesthetic protocols. Some diabetic patients report unusual sensations during catheter manipulation that differ from typical procedural experiences. Clear communication between patients and procedural teams helps distinguish between expected sensations and concerning symptoms requiring intervention.
Anxiety disorders and vasovagal response management
Patients with pre-existing anxiety disorders require specialised approach to catheterisation comfort management. Anxiety can amplify pain perception and create a cycle of increasing distress during procedures. Early identification of anxious patients allows implementation of enhanced comfort protocols, including increased sedation, additional reassurance, and modified procedural techniques.
Vasovagal responses, characterised by bradycardia and hypotension, can occur in susceptible patients during catheterisation. These responses often correlate with anxiety levels rather than actual procedural pain. Prophylactic measures, including adequate hydration and premedication, can prevent most vasovagal episodes and maintain patient comfort throughout the procedure.
Recovery timeline: immediate Post-Catheterisation monitoring and discharge protocols
The immediate recovery period following cardiac catheterisation typically spans 2-6 hours, depending on the access site used and procedural complexity. Monitoring protocols focus on access site assessment, vital sign stability, and pain management during this critical period. Most patients experience minimal discomfort during recovery, with pain scores remaining consistently low throughout the observation period.
Access site monitoring includes regular assessment for bleeding, haematoma formation, and distal pulse evaluation. Nursing staff perform these checks every 15-30 minutes initially, gradually extending intervals as stability is demonstrated. Patient education regarding activity restrictions and signs requiring medical attention forms a crucial component of discharge preparation.
Pain management during recovery utilises multimodal approaches, combining oral analgesics with non-pharmacological comfort measures. Ice application to access sites reduces swelling and provides analgesic effects, while positioning adjustments maintain comfort during observation periods. Most patients require only minimal analgesia, typically paracetamol or ibuprofen, for post-procedural comfort.
Discharge criteria include haemodynamic stability, absence of significant bleeding, adequate pain control, and patient understanding of post-procedural instructions. The majority of catheterisation patients meet these criteria within 4-6 hours for femoral access and 1-2 hours for radial access. Outpatient catheterisation has become the standard of care , with overnight admission reserve
d for complex cases or patients with comorbidities requiring extended observation.
Patient education during the recovery phase emphasises recognising normal healing sensations versus complications requiring medical attention. Mild soreness at the access site is expected and typically resolves within 24-48 hours. However, increasing pain, swelling, or changes in pulse strength warrant immediate evaluation. Clear discharge instructions with specific parameters for seeking medical care help patients manage their recovery confidently at home.
Activity restrictions following catheterisation vary based on access site and procedural complexity. Femoral access patients typically avoid heavy lifting and strenuous activity for 24-48 hours, while radial access allows almost immediate return to normal activities. Driving restrictions depend on sedation use and overall recovery status, with most patients cleared for driving within 24 hours of uncomplicated procedures.
Follow-up appointments are scheduled based on procedural findings and treatment plans. Diagnostic catheterisation may require only routine cardiology follow-up within 1-2 weeks, while therapeutic interventions necessitate closer monitoring. Pain or discomfort during the recovery period rarely indicates serious complications but should be communicated to the healthcare team for appropriate guidance and reassurance.
The overwhelming majority of patients report that cardiac catheterisation was far more comfortable than anticipated, with most describing the experience as “easier than expected” and recommending the procedure to others facing similar cardiac evaluation.
Long-term comfort outcomes following catheterisation are excellent, with most patients experiencing complete resolution of access site discomfort within one week. The procedure’s minimally invasive nature means that ongoing pain or functional limitations are extremely rare. Modern catheterisation techniques have evolved to prioritise patient comfort without compromising diagnostic accuracy or therapeutic efficacy, making this essential cardiac procedure accessible and tolerable for virtually all patients requiring cardiovascular evaluation or treatment.

 Good health cannot be bought, but rather is an asset that you must create and then maintain on a daily basis.
Good health cannot be bought, but rather is an asset that you must create and then maintain on a daily basis.
